Brain Research, Innovation & Translation Laboratory (BRITL)
Hawaii Pacific Neuroscience is recognized nationally for our work in neuroscience research conducted at the Clinical Research Center and BRITL (Brain Research, Innovation & Translation Labs). HPN’s robust clinical and academic research programs fosters a culture of innovation and collaboration. Physicians and scientists work closely within and across centers, institutes, and schools to collaborate whether they are basic laboratory-based scientists, bio statisticians or clinicians to encourage cross disciplinary translation bench to bedside research.
The BRITL Neuroscience research program is part of the University of Hawaii John Burns School of Medicine MD5 MED 599 Neuroscience Research Course. University Hawaii medical students may sign up for elective credit while working at BRITL in MD5 MED 599 Neuroscience research credit. Inquire with David Horio, MD dhorio@hawaii.edu
HPN accepts a number of “Hawaii BRITL Neuroscience Scholars” each year to work with our neurology & neuroscience research faculty on various projects each year on groundbreaking studies in Alzheimer’s disease, epilepsy, Parkinson’s disease, multiple sclerosis, and other neurological diseases.
BRITL’s mission is to support our local medical students to pursue their passion in neuroscience, research and develop leadership in this field to make an impact in the local community. It provides students the opportunity to work in a team setting working with seasoned investigators, junior investigators, residents, senior student leaders and junior students. This team will also recruit graduate and undergraduate students to be part of the team for summer internship projects.
HPN is proud to recognize exceptional medical students as “neuroscience academic scholars” and project leaders who have demonstrated exemplary academic abilities in neuroscience, leadership qualities, passion, and commitment to the pursue of excellence in research and a commitment to make a difference in the local and global community.

Core Neurology/Neuroscience Faculty
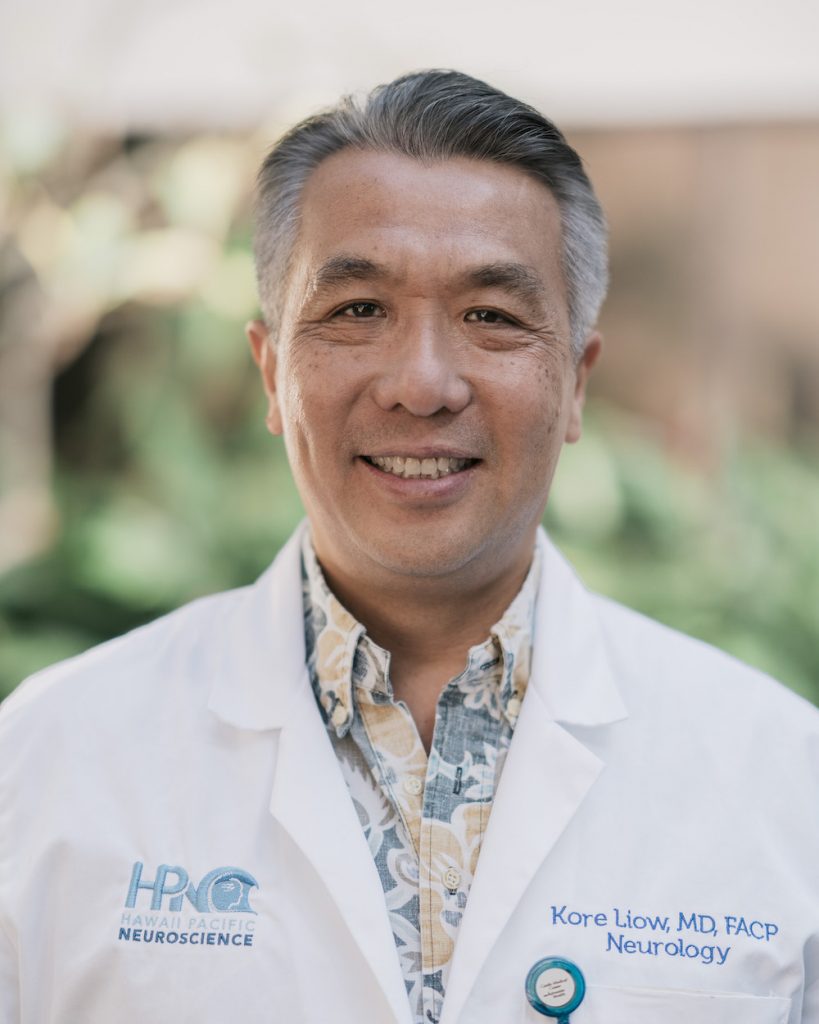
Academic Director,
Assistant Professor
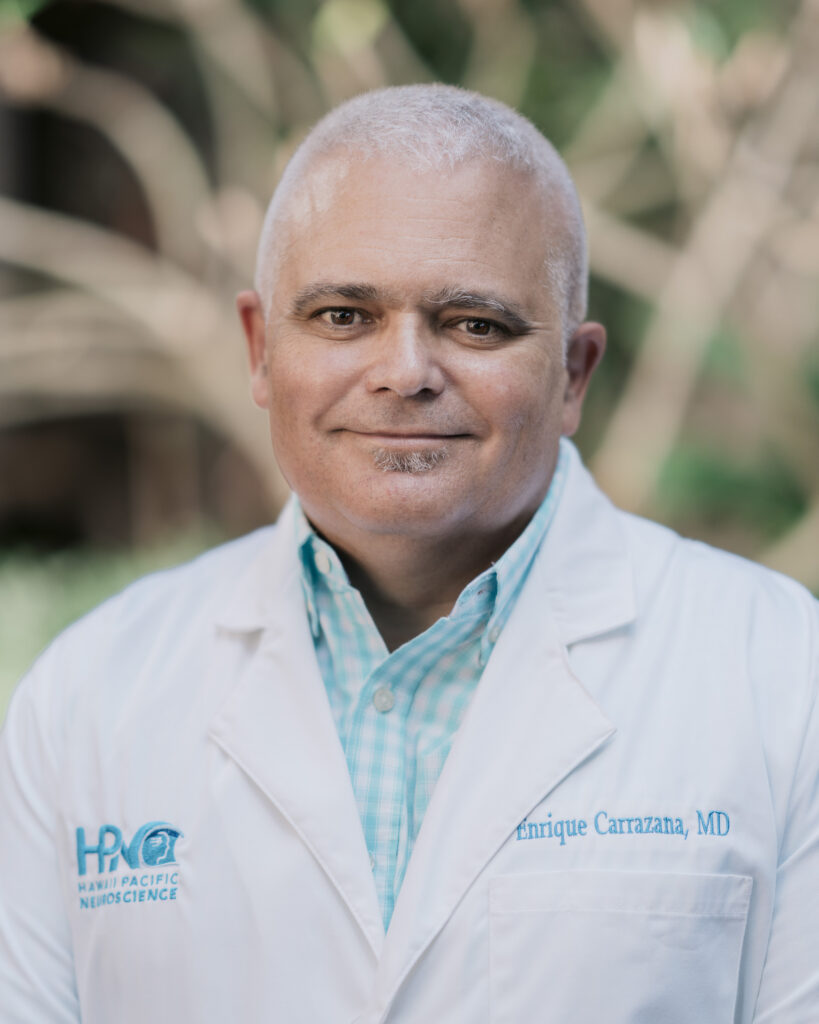
Enrique Carrazana, MD
Publications Director,
Clinical Educator

Janette Abramowitz, MD,
Assistant Professor

Eliza Hagen, MD
Neurology
Core Biostatistics & Research Faculty

John Chen, PhD
Professor & Chair, Dept. Quantitative Health Sciences

Chathura Siriwardhana, PhD
Assistant Professor and Biostatistician

Lawrence Burgess, MD

Russell Woo, MD
Professor and Director of Medical Student Research
Brain Research, Innovation & Translation Labs (BRITL)
2230 Liliha Street #104, HONOLULU, HI 96817
June 17th-August 5th, 2023
June 17th Sat ORIENTATION Spring Presentation
Myasthenia Gravis Symposium Register Online

Introduction
Kore Kai Liow, MD
Neuroscience ChairClinical Professor Medicine (Neurology)
Graduate Faculty, Clinical & Translational Research

Visiting Professor Keynote Speaker
Richard Nowak, MD, MS
Neuroscience ChairDirector, Yale Myasthenia Gravis Clinic
Director, Program in Clinical & Translational Neuromuscular Research,
Assistant Professor of Neurology, Yale University School of Medicine
June 20, 27 Tues
5:00-6:30PM

Research Bio Statistics I and II
Chathura Siriwardhana, PhD,
Assistant Professor,Biostatistics Core Facility,
Dept. Quantitative Health Services
July 8th Saturday

MID TERM Oral Presentation
Keynote Speakers
Jason Viereck, MD, PhD
Academic Director, BRITL,Clinical Assistant Professor of Med (Neurology)
July 11 Tues
5:00-6:00PM

Writing up Your Abstract and Poster
Enrique Carrazana, MD
Publication Director, Neurology, Hawaii Pacific Neuroscience, Clinical EducatorJuly 18th, 25th -Tues
5:00-6:00PM



How to Get Your Posters Ready
How to Submit to National Meetings
How to Submit for Full length Publications
Julia Jahansooz, MS3
Ward Weldon, MS3
Anson Lee, MS3
2023 BRITL Academic Scholars & Leaders
Aug 19th Sat
9-2:00PM
FINAL Poster Presentation

Native Hawaiian & Pacific Islanders Health Disparity
Keaweʻaimoku Kaholokula, PhD
Professor and Chair of Native Hawaiian Health, John A. Burns School of Medicine
Visiting Professor Keynote Speaker
Advances in Spasticity, Dystonia & Blepharospasm Treatments
Zoltan Mari, MD
Ruvo Family Chair for Parkinson’sDisease & Movement Disorders
Lou Ruvo Center for Brain Health, Cleveland Clinic


Presentation Research Award
2023 HI Neuroscience Best Posters Presentations
Lawrence Burgess, MD
Director, Student AffairsRussell Woo
MD Associate Director of Research2022-2023 Hawaii BRITL Project Leaders
 Julia Jahansooz graduated from the University of California, Berkeley with a degree in Integrative Biology. She went on to earn her master’s degree in Clinical and Translational Research from the University of Hawai’i and is now a second year medical student at JABSOM. Julia believes research is the backbone of clinical practice and encourages everyone to participate in some level of research during their career.
Julia Jahansooz graduated from the University of California, Berkeley with a degree in Integrative Biology. She went on to earn her master’s degree in Clinical and Translational Research from the University of Hawai’i and is now a second year medical student at JABSOM. Julia believes research is the backbone of clinical practice and encourages everyone to participate in some level of research during their career.  Ward Weldon graduated from Punahou Highschool and earned a Bachelor of Science in Biology at the Massachusetts Institute of Technology (MIT). He is currently a second year medical student at JABSOM. Ward recommends that interested medical students engage in research early in their careers, so they may develop the skills to lead meaningful research in the future as physicians.
Ward Weldon graduated from Punahou Highschool and earned a Bachelor of Science in Biology at the Massachusetts Institute of Technology (MIT). He is currently a second year medical student at JABSOM. Ward recommends that interested medical students engage in research early in their careers, so they may develop the skills to lead meaningful research in the future as physicians. 2022-2023 Hawaii BRITL Student Editor
 Anson Lee graduated from Punahou School and went on to earn a B.S. in Molecular and Cellular Biology, B.A. in Archaeology, and B.A. in Near Eastern Studies at Johns Hopkins University. Currently, he is a second-year medical student at the JABSOM. Anson believes that participating in research is the best way to improve patient care and lead the future of medical practice.
Anson Lee graduated from Punahou School and went on to earn a B.S. in Molecular and Cellular Biology, B.A. in Archaeology, and B.A. in Near Eastern Studies at Johns Hopkins University. Currently, he is a second-year medical student at the JABSOM. Anson believes that participating in research is the best way to improve patient care and lead the future of medical practice. 
Medical students: Anita Cheung (lead), D-Dre Wright (lead), Erin Kim, Lauren Kim, Ryan Nishi, Jiwoo Kim






Differences in Neuropathy Etiology, Presentation & Treatment in AANHPI Populations
● To identify etiological trends of neuropathy especially in AANHPI populations
● To identify differences in clinical presentation and treatment of neuropathy in the AANHPI population compared to other ethnocultural groups in Hawaii
● To identify associated comorbidities in AANHPI populations
Risk Factor Association of Diabetic Neuropathy
● To assess prevalence of diabetic neuropathy in NHPI populations compared to other populations
● To analysis the relationship between diabetes and peripheral neuropathy especially in NHPI populations
Medical students: Ryan Nakamura (lead), Erin Evangelista

 TBI Education
TBI Education
• Concussion education and awareness has been a sustained effort in neurology since the first understanding of concussive injuries
• To survey high schools, colleges, and medical students about their respective understandings and perceptions of concussions

Medical students: Shay Nakahira (lead), Kirra Borrello (lead), Kylie Yamauchi, Janette Bow-Keola




Investigating Neural Network using EEG for early detection and monitoring of Alzheimer’s Disease
• To investigate the possibility of using EEG as a potential non-invasive biomarker to facilitate early detection and intervention/management of Alzheimer’s Disease
• Evaluate P300 latency and amplitude in ApoE4+ vs. ApoE4- and CSF+ vs. CSF-
• Analyze P300 changes over time in ApoE4+/- and CSF+/-
Medical students: Ryan Nakamura (lead), Michaela Kop, Anna Gan



Evaluating the Onset of Falls and Fall Frequency in Mild Cognitive Impairment – a Case Control Study
• To determine the odds ratio of falls vs. MMSE scores and observe if the onset of falls is sooner than the cognitive decline
• To evaluate whether patients living with dementia who are at high fall risk, suffer more frequent
traumatic brain injuries
Medical students: Cierra Nakamura (lead), Liza Rooks (lead), Kaela Iwai, Tyrone John Sumibcay, Matthew Kao, Megan Kawamura






Characterizing Epilepsy in Native Hawaiian and Pacific Islander Populations
• Characterize the severity of epilepsy in NHPI population, treatment course and outcomes
• How do NHPI patients with epilepsy present?
Smoking and Risk for Depression in People with Epilepsy
• Investigate the relationship between depression, nicotine use, and epilepsy severity by:
• Examining the prevalence of depression in individuals who are smokers, former smokers, and non-smokers
• Investigating the correlation between the length of smoking history and the presence of seizures, refractory epilepsy status, and epilepsy-related quality of life
Medical students: Bradon Hong (lead), Justin Wong, Sarah Bellati



Prevalence of Small Vessel Disease in NHPI Stroke Patients
• Current literature show that NHPI patients are 4x more likely to suffer a stroke than non-Hispanic white adults
• To examine the prevalence of cerebral small vessel disease (CSVD) in NHPI compared to other ethnic groups in Hawaii, including Caucasians, Asians, and African Americans

Medical Students: Johnny Carino (lead), Nina Krupa, Anna Davide



A Comprehensive Analysis of Depression Screening Practices in MS Outpatient Care
• To evaluate the applicability and routine implementation of the PHQ-2/9 depression screening tool in an outpatient MS clinic
• To map the patient journey from post-screening, focusing on referral patterns and management
Questions ? contact Principal Investigator Kore Kai Liow, MD kliow@hawaii.edu
Residents or students interested in working in neuroscience research should visit below –
Brain Research, Innovation, Translation Labs.
Summer Internship Opportunities